Diabetic Retinopathy
We are continuing to care for our patients both in our clinic and in surgery. We are accepting new patients and appointments are available.
We are continuously cleaning/disinfecting patient contact areas, and our building is professionally cleaned and disinfected multiple times a week. We have installed plexiglass partitions at our front desk. UV-C light sterilizing units have been installed in all our HVAC units to sterilize all circulating airflow in the building. UV-C portable units are also being utilized to sterilize equipment and individual rooms.
During the ongoing COVID-19 pandemic, our utmost priority is your health and well-being.
Masks are optional.
If you have diabetes, it is important to know that today, with improved methods of diagnosis and treatment, a smaller percentage of people who develop retinopathy have serious vision problems. Early detection of diabetic retinopathy is the best protection against vision loss.
There are two types of diabetic Retinopathy
Nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR)
NPDR, also known as background retinopathy (BDR), is an early stage of diabetic retinopathy. In this stage, small blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates.
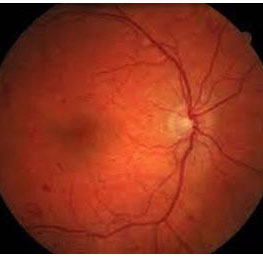
Early background diabetic retinopathy (BDR)
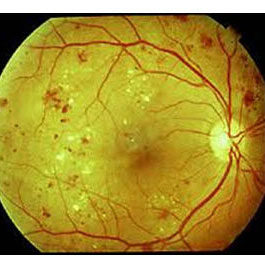
Moderate diabetic retinopathy (NPDR)
Many people with diabetes have mild NPDR which usually does not affect their vision. When vision is affected it is usually the result of macular edema (swelling) or macular ischemia.
Macular edema is swelling or thickening of the macula, a small central area of the retina that allows us to see fine details clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe.
Macular ischemia occurs when small blood vessels close. Vision blurs because the macula no longer receives enough blood to work properly.
PDR is present when abnormal new blood vessels (neovacularization) begin growing on the surface of the retina and or optic nerve. The main cause of the PDR is extensive closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where vessels have closed. However, the new abnormal vessels do not resupply the retina with normal blood flow. The new abnormal blood vessels leak and bring scar tissue that may lead to retinal detachment and hemorrhage (bleeding).
 PDR may cause more severe vision loss than NPDR because it can affect both central and side vision.
PDR may cause more severe vision loss than NPDR because it can affect both central and side vision.
Proliferative diabetic retinopathy (PDR)
PDR causes visual loss by:
Vitreous hemorrhage. The fragile new blood vessels may bleed into the vitreous, a clear gelatinous substance that fills the center of the eye. If the vitreous hemorrhage is small, a person might see only a few new floaters. A large hemorrhage might block all vision. It may take days, months or even years to reabsorb the blood. If the eye does not clear the vitreous blood within a reasonable time, vitrectomy surgery may be performed. The vitreous hemorrhage alone does not cause permanent vision loss. However, when the blood clears, either by reabsorbing or surgical vitrectomy the amount of vision return will be determined by the extent of retinal damage.
Tractional retinal detachment. When PDR is present, scar tissue can form with the neovascularization and cause wrinkling and contraction of the retina from its normal position. Macular wrinkling can cause visual distortion. Further contraction can lead to severe vision loss due to retinal detachment.
Neovascular Glaucoma. PDR can lead to abnormal blood vessels plugging the normal flow of fluid out of the eye leading to greatly elevated eye pressure. As the pressure builds extensive damage can occur to the optic nerve and lead to permanent loss of vision.
How do you know you have Diabetic Retinopathy?
An ophthalmologist can diagnose and treat diabetic retinopathy before you are aware of any vision problems. The ophthalmologist dilates your pupils and looks inside your eyes with special lenses. If your ophthalmologist finds diabetic retinopathy, he may order color photographs of the retina to better follow the progression. He may also perform a test called fluorescein angiography to locate treatable leakage points. Optical Coherence Tomography (OCT) is commonly performed. It gives a detailed 3D image of your retina.
Is diabetic retinopathy treatable?
The best treatment is prevention. Diabetic patients need strict control of blood sugar, blood pressure and cholesterol. This will significantly decrease the long-term risk of vision loss from diabetic retinopathy. If early diabetic retinopathy is present, only lifestyle changes such as eating better and blood pressure control may be sufficient in preventing progression. However, periodic eye examinations with your ophthalmologist are vital in determining whether the disease is controlled.
If macular edema is significant or if neovascularization is present, there are treatments available
Injections. Injections of anti-VEGF medication (Lucentis, Avastin, Eylea, Macugen) in the eye can stop the growth of new blood vessels and cause regression of already formed abnormal vessels. Sometimes a steroid medication may be used. These injections are widely used. Anti-VEGF injections are also used to decrease macular edema.
Laser surgery. Laser surgery is often recommended for people with macular edema, PDR and neovascular glaucoma, many times in conjunction with anti-VEGF injections.
For macular edema, the laser is focused only on specific areas of the macula that are leaking. For PDR and neovascular glaucoma, the laser is focused throughout the peripheral retina. This panretinal photocoagulation prevents vessels from regrowing.
Vitrectomy. In advanced PDR, your ophthalmologist may recommend a vitrectomy. During this surgical procedure, the blood filled vitreous is removed and replaced with clear solution. Also, scar tissue may be removed and laser performed. Vitrectomy often prevents further bleeding by removing the abnormal blood vessels. If the retina is detached, it can be repaired during vitrectomy surgery. Surgery should be done in a timely fashion because macular distortion or traction retinal detachment will cause permanent visual loss.
You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar, blood pressure and cholesterol. Also, it is vital to visit your ophthalmologist regularly for dilated eye examinations.
